Osteoarthritis is a chronic disease of the joints that is accompanied by pathological changes in the hyaline cartilage and then in the adjacent tissues, the joint capsule and the synovia.
The lesion is dystrophic and degenerative, which leads to a change in the structure of the joint tissue and a loss of its functionality. According to the same statistic, 12% of the total population of the planet is prone to osteoarthritis. 62% to 65% of all episodes of the disease occur in people over the age of 60.
Another 30-35% of cases of joint damage with this pathology occur in patients aged 40-60 years. And around 3% are young people between the ages of 20 and 40.
What is that?
In simple terms, osteoarthritis is a chronic disease in which progressive degenerative-dystrophic changes develop in the joint due to metabolic disorders. It is the most common joint pathology diagnosed in 6-7% of the population. The incidence increases dramatically with age.
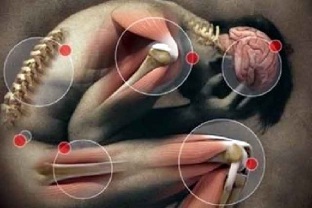
Most often, the pathological process in osteoarthritis affects the small wrists (ten times more often in women than in men), the big toe, the intervertebral joints of the thoracic and cervical spine, and the knee and hip joints. Osteoarthritis of the knee and hip joints takes the top spot in terms of the severity of clinical manifestations and the negative impact on quality of life.
Osteoarthritis is characterized by a complex lesion of the joint and auxiliary apparatus:
- Chondritis - inflammatory changes in the cartilage of the joint;
- Osteitis - involvement of the underlying bone structures in the pathological process;
- Synovitis - inflammation of the inner membrane of the joint capsule;
- bursitis - damage to the periarticular sac;
- reactive inflammation of soft tissues (muscles, subcutaneous tissue, ligamentous apparatus) in the projection of the affected joint (periarticular inflammation).
The disease is diagnosed in 2% of people under 45 years of age, in 30% - from 45 to 64 years and in 65-85% - at the age of 65 and older. Osteoarthritis of the large and middle joints of the extremities has the greatest clinical significance due to its negative impact on the standard of living and the ability to work of patients.
Types of osteoarthritis
Depending on the cause of the pathological process in the joint, a distinction is made between primary osteoarthritis, secondary and idiopathic.
Primarily develops as a disease in its own right, secondary, as a result of injury or infection, and the cause of the idiopathic form is unknown. In addition to the classification of the disease, depending on the cause of the pathological process, osteoarthritis is distinguished according to the location of the destructive changes:
- Gonarthrosis is the most common type of pathology, which is characterized by damage to the knee joints. Most often, osteoarthritis of the knee is noted in overweight people with chronic metabolic diseases in the body and poor immunity. Knee osteoarthritis progresses for a long time and gradually leads to a complete loss of motor skills.
- Osteoarthritis of the shoulder joint - the main cause of degenerative processes in this area is congenital abnormalities in the development of the shoulder joint or excessive load on this area, for example, when carrying heavy luggage on the shoulders.
- ankle arthrosis - the main reasons for the development of degenerative processes in the ankle are trauma, sprains, sprains and fractures. In some cases, the development of a pathological process can provoke an autoimmune disease - rheumatoid arthritis. Ankle osteoarthritis affects dancers, high-heeled women, and athletes.
- Uncoarthritis or osteoarthritis of the cervical spine - the causes are neck injuries, progressive osteochondrosis, obesity and a sedentary lifestyle. People who work on computers in offices are at risk. In addition to severe neck pain, patients experience pronounced dizziness, depression of consciousness, impaired memory, and fatigue. These symptoms are caused by the compression of the vertebral artery, which allows nutrients and oxygen to enter the brain.
- Coxarthrosis or osteoarthritis of the hip joint - the main cause of its occurrence is age-related changes in the tissue of the joint. People over 45 are at risk.
- Osteoarthritis of the fingers - develops for the same reason as spondyloarthrosis.
- Polyarthrosis is characterized by damage to multiple joints with progressive degenerative processes, while the pathological process involves ligaments, muscles, and tissues that surround the joint.
- Spondyloarthrosis - the tissues of the spine, namely your lumbar region, are exposed to destructive destruction. Women are at risk during menopause, as spondyloarthrosis progresses against the background of a lack of female sex hormones.
Causes of osteoarthritis
Two reasons contribute to the development of osteoarthritis - stress and lack of adequate nutrition, which provides vitamins and minerals for tissue repair. Every person's joints carry a load. For athletes and dancers, the load on the legs is greater during physical work, which means that the bone joints wear out faster and require quality nutrition. In a calm lifestyle, the supporting apparatus wears out more slowly, but also requires regular tissue renewal.
Therefore, the main condition for the destruction and deformation of the joints is malnutrition, the digestive disorder of useful components, which often occurs with metabolic disorders.
Let's list the factors that contribute to joint wear and tear and metabolic disorders:
- Muscle weakness and abnormal stress on the joints. Weakening one or more muscles increases the stress on the joint and distributes it unevenly within the bone junction. The wrong muscle strain is also created with flat feet, scoliosis, which is why the cartilage tissue of these "harmless" diseases wears out with age, and osteoarthritis occurs.
The probability of osteoarthritis increases with intense physical exertion.
When the daily loads exceed the capacity of the bone tissue, a microtrauma forms in them. Thickenings appear at the injury sites, which over time grow and deform the joint;
- Metabolic disorders (gastrointestinal diseases - stagnation of bile, dysbiosis, gastritis, cholecystitis, pancreatitis, metabolic disease - diabetes);
- Psychosomatic causes - The psychosomatics of osteoarthritis confirms that a negative emotional state also becomes the cause of the disease. Stress creates muscle spasms, constant stress disrupts the nutrition of all tissues (internal organs, bones, joints);
- Heredity (the nature of the metabolism and its possible disorders are inherited, a tendency to muscle weakness or improper formation of the bone structure, poor digestion - which is the basis for the development of osteoarthritis in old age).
Osteoarthritis is a condition of worn joints that have lost significant supplies of minerals and the ability to withstand stress and destruction. Therefore, the predisposition to the disease increases with age. After 70 years, every second pensioner is diagnosed with osteoarthritis. Since the maximum load falls on the legs (a person moves - walks, stands, runs, jumps), this is where the first signs of osteoarthritis are formed.
Mechanism of the course of the disease
If any of the causes of joint disease with osteoarthritis occurs, then pathological processes in it begin to develop. The mechanism of their progression is not fully understood, but the main stages of official medicine are known.
In the initial stage, the structure of the cartilage tissue becomes exhausted and there are abnormal changes in the synovial fluid. All of this happens due to metabolic disorders, in which the tissues of the joints do not receive the necessary components in sufficient quantities or do not contain some of them.
Furthermore, the elasticity of the collagen fibers and the flexibility of the cartilage are lost, since hyaluronic acid in the body with a lack of nutrients has no time to produce, which ensures the softness and flexibility of the structural composition of the collagen fibers. The cartilage gradually dries out, becomes brittle and cracks. The fluid in the synovial capsule is gradually used up and then disappears completely.
Roughness and solid bone growth form on the cartilage tissue. At the same time, deformation of other articular tissues develops, their pathological degeneration, dystrophy and loss of physiological activity. For the patient, these changes mean the occurrence of pain, lameness and joint stiffness.
Symptoms of osteoarthritis
Acute clinical picture is not typical for osteoarthritis, joint changes are progressive and increase slowly, which is expressed in a gradual increase in symptoms:
- pain;
- intermittent grinding of the affected joint;
- joint deformity that occurs and worsens as the disease progresses;
- stiffness;
- Restriction of mobility (reduction in the volume of active and passive movements in the affected joint)
Osteoarthritis pain is dull, transient, and occurs when you move around against a background of intense stress towards the end of the day (it can be so intense that the patient cannot fall asleep). The constant, non-mechanical nature of pain in osteoarthritis is atypical and indicates the presence of active inflammation (subchondral bone, synovium, ligamentous apparatus, or periarticular muscles).
Most patients notice the presence of so-called start-up pains, which appear in the morning after waking up or after a long period of inactivity and which go away during physical activity. Many patients define this condition as the need to develop or loosen a joint.
Osteoarthritis is characterized by morning stiffness, which has a clear localization and is of a short-term nature (no longer than 30 minutes). Sometimes it is perceived by patients as a "feeling of gel" in the joints. Wedge feeling, stiffness is possible.

With the development of reactive synovitis, the following main symptoms of osteoarthritis are added:
- Pain and local temperature rise, determined by palpation of the affected joint;
- persistent pain;
- enlargement of the joint, swelling of the soft tissue;
- progressive decrease in the range of motion.
Stages and degree of osteoarthritis
In the course of the disease, medicine distinguishes three stages, which differ in the signs of the disease, the intensity of the lesion and the localization. At the same time, the differences in all three stages relate to the types of tissue that are subject to pathological changes.
- The first stage in the development of osteoarthritis of the joints is the initial phase of the disease. It is characterized by slight damage to the cartilage tissue and loss of physiological functions in collagen fibers. At the same time, in the first stage, minor morphological disorders of the bone tissue and structural changes in the synovial fluid are noted. The cartilage of the joint is covered with cracks, the patient has slight pain in the place of the pathology.
- Second degree - the development of osteoarthritis with increased dynamics. This stage is characterized by the appearance of stable pain and lameness. There are noticeable morphological and dystrophic changes in cartilage, during the diagnosis, the growth of bone tissue is revealed. Osteophytes are formed - bone growth that can be seen when visually examining the site of the lesion. At the same time, the processes of degenerative changes take place in the synovial capsule, which leads to its structural exhaustion. The disease at this stage can often get worse and occur regularly. The pain gradually becomes constant.
- Third degree - active progression. At this stage, the synovial fluid is almost completely absent due to its degeneration, and the bone tissue is rubbed together. The mobility of the joints is almost completely absent, the pain becomes more noticeable. Cartilage is also absent due to degenerative and atrophic changes. Treatment of the third degree of osteoarthritis of the joints is considered inappropriate.
In addition to these three stages of development of the pathology, there is an end stage - the irreversible destruction of all tissues in the joint. At this stage it is impossible not only to carry out effective therapy, but also to relieve pain.
The inflammatory process usually begins in the second degree of the lesion, in rare cases without medical intervention - in the first stage. As a result, it becomes more and more difficult to stop it, and this can lead to secondary pathologies, the development of a pathogenic microflora instead of the localization of the disease.
In order to exclude serious consequences, treatment should be started from the first degree, and at the same time intensive methods of therapy should be used. In the last stage, which is associated with the complete destruction of the cartilage tissue, only one technique is allowed to relieve the patient of pain and immobility of arthroplasty of the joint, completely or partially replacing the components of the joint.
Follow
The consequences of early treatment and advanced osteoarthritis of the joints are accompanied by complications such as
afflicted- handicap;
- deformation until recovery;
- Occurrence of vertebral hernias;
- joint stiffness or stiffness;
- Decline in quality of life and standard of living.
The chronic course, in addition to these complications, is accompanied by severe and frequent pain, complete destruction of the structural components of the joint, discomfort, inability to do physical work and play sports.
diagnosis
The diagnosis of osteoarthritis is based on the assessment of anamnestic data, characteristic manifestations of the disease and the results of instrumental research methods. Indicative changes in general and biochemical blood tests are not typical of osteoarthritis, they appear only with the development of an active inflammatory process.
The most important instrumental method for diagnosing osteoarthritis is radiography. In diagnostically unclear cases, a calculated or magnetic resonance tomography is recommended.
Osteoarthritis of the knee and hip joints plays a leading role in the severity of clinical manifestations and the negative effects on quality of life.
Additional diagnostic methods:
- atraumatic arthroscopy;
- Ultrasound (assessment of the thickness of the articular cartilage, synovia, the condition of the joint capsules, the presence of fluid);
- Scintigraphy (assessment of the condition of the bone tissue of the heads of the bones that make up the joint).
How do you treat osteoarthritis?
It is better to treat osteoarthritis of the joints early. Treatment itself should be pathogenetic and complex. Its essence lies in eliminating the causes that contribute to the development of this disease. It is also necessary to get rid of inflammatory changes and restore previously lost functions.
The treatment of osteoarthritis is based on several basic principles:
- Oxygen supply to the joint or so-called intra-articular oxygen therapy.
- drug therapy.
- Intraosseous blockages and decompression of the metaepiphysis.
- Sustainable nutrition.
- Damaged joints must be relieved of excessive stress. If possible, it should be kept to a minimum during treatment.
- Follow the established orthopedic scheme.
- Physiotherapy exercises.
- Take a physical therapy course that includes magneto and electrotherapy, shock wave and laser therapy.
- sanatorium treatment. For this purpose, on the recommendation of a doctor, treatment must be carried out once a year in specialized resorts.
Preparations for the treatment of osteoarthritis
Drug treatment is carried out in the phase of exacerbation of osteoarthritis selected by a specialist. Self-medication is not acceptable due to possible side effects (e. g. the negative effect of non-steroidal anti-inflammatory drugs on the gastric mucosa).
Therapy includes the following drugs:
- Anti-inflammatory drugs. If you start osteoarthritis therapy comprehensively, you can slow down the course of the disease and significantly improve the quality of life. It is worthwhile to go into some treatment points in more detail. Drug therapy includes, especially at the initial stage - this is the elimination of pain, as well as the elimination of inflammatory processes in the joints. For this purpose, all doctors use nonsteroidal anti-inflammatory drugs. Experienced doctors do not recommend oral administration because these drugs are very irritating to the stomach wall. Therefore, either intravenous or intramuscular administration is used depending on the drug chosen. Sometimes NSAIDs are used as an aid in the form of ointments, but their absorption is extremely low, so no significant effect can be achieved.
- hormonal corticosteroids. If the osteoarthritis is in the exacerbation stage, it is advisable to take hormonal corticosteroids. They are injected into the joint. Externally, you can use a special patch, ointment or tincture made on the basis of paprika.
- Chondroprotectors to restore the cartilage and improve the qualitative composition of the synovial fluid are not superfluous. The course takes a long time to improve. However, if the expected effect does not appear within six months after administration, the drugs should be canceled. In addition to chondroprotectors, it is also advisable to use medicines that are made on the basis of hyaluronic acid. They contribute to the formation of the cell membrane, which is responsible for the formation of articular cartilage.
Physiotherapy
To relieve pain, reduce inflammation, improve microcirculation and relieve muscle spasms, a patient with osteoarthritis is referred for physiotherapy:
- In a worsening phase. Prescribe laser therapy, magnetotherapy, and ultraviolet radiation,
- In remission. Electrophoresis and phonophoresis shown.
In addition, thermal processes, sulfide, radon and marine baths are used. Electrical stimulation is performed to strengthen the muscles. A gentle massage can also be used during remission.
surgery
If the listed influencing methods are ineffective, resort to surgical treatment of osteoarthritis in the event of complications:
- Decompression of the metaepiphysis and prolonged intraosseous blockade (decrease in intraosseous pressure in the affected area);
- Corrective osteotomy;
- Endoprosthetics of joints.
In the early stages of the disease, mechanical debridement, laser or cold plasma debridement (smoothing the surface of damaged cartilage, removing non-viable areas) is used. This method is effective in relieving pain, but has a temporary effect - 2-3 years.
folk remedies
Most people nowadays don't want to take pills or injections anymore. Therefore, they ask the question: how to cure osteoarthritis with the help of folk remedies? For the most part, these funds are aimed at improving the tone of the body, improving blood circulation, relieving pain and strengthening immunity.
Traditional medicine recipes are used to treat this disease:
- egg solution is made from fresh egg yolk mixed with turpentine and apple cider vinegar in a ratio of 1: 1: 1. The liquid must be mixed thoroughly and rubbed over the affected joint overnight. Then you need to wrap everything in a woolen scarf. It is recommended to rub 2-3 times a week for 1 month.
- Buy the Elecampane root in the pharmacy. It is usually packaged in packs of 50 grams. To prepare the tincture, you need half a pack of plant roots and 150 ml of high-quality vodka. The ingredients are mixed, placed in a dark bottle and infused for 12 days. Rubbing is done before going to bed and, if possible, in the morning.
- Using cooked oatmeal also gives good results. Take three to four tablespoons of oatmeal, pour boiling water over it and cook over low heat for five to seven minutes. The amount of water used should make a thick gruel that should be cooled and used as a compress overnight. Use only freshly cooked flakes. Yesterday's porridge is not good for a compress.
- Birch leaves, nettle leaves and marigold inflorescences are taken in equal parts. As a result, you will need two tablespoons. We put the resulting crushed collection in a thermos, fill it with a liter of boiling water and let it stand overnight. From the next morning, you need to take half a glass of the broth four to five times a day. This recipe takes two to three months to take.

Tinctures made from bay leaves, horseradish, garlic and rye are also considered effective. Treatment of osteoarthritis with folk remedies is most effective when combined with medication.
Diet for osteoarthritis
The basic principles of nutrition in osteoarthritis are reduced to the following points:
- Avoid heavy meals at night to avoid an attack of osteoarthritis.
- Eat Fractional.
- Constantly monitor your weight in order to avoid weight gain,
 and thus additional stress for painful joints.
and thus additional stress for painful joints. - If the disease doesn't get worse, take a walk after you eat.
- The menu must be balanced and created with the treating physician.
There are absolutely no complaints about fish dishes - you can of course eat many of them in reasonable amounts.
- Do not forget the regular intake of vitamins from food. For patients with osteoarthritis, vitamins of group B are particularly relevant
- Gelled meat plays an important role in treating osteoarthritis. Such foods will be a real storehouse of trace elements for sore joints. The most important component in aspic is naturally occurring collagen
- Vitamin B helps in the production of hemoglobin. It can be "obtained" by eating bananas, nuts, cabbage and potatoes. It is worth getting carried away with herbs and legumes. They will be the source of folic acid. Liver, mushrooms, dairy products and eggs are useful. They are high in riboflavin.
According to the treatment regimen prescribed by the doctor, it can be achieved that the disease regresses and the damaged tissue begins to regenerate.
Prevention
The prevention of osteoarthritis begins with the right diet. It is necessary to try to reduce the intake of salt, as well as foods that can disturb the metabolism. These include legumes, fatty meat, and alcohol. The diet includes cabbage, vegetables, and fish.
To prevent osteoarthritis, it is necessary to take physical education classes and do warm-up exercises. If possible, it is better to run a few kilometers. It is also important to monitor your weight and prevent weight gain as this will put additional strain on the sore joints. It is not recommended to take pills for weight loss as they can disrupt the metabolism in the body.
forecast
The prospects for life are good. The feasibility of the social and work prognosis depends on the timeliness of the diagnosis and the start of treatment and decreases if the decision on the question of surgical treatment of the disease is delayed.





































